What We Can Do For You
Services
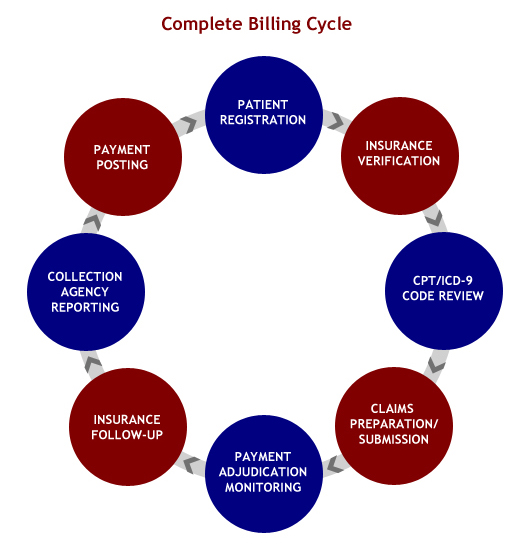
Billing Concepts Inc. provides client-focused medical billing solutions in minimum turnaround time. We are staffed with skilled medical billing experts, Certified Coders and quality controllers. We are well informed about the latest changes in billing, coding and claims professing norms and offer customized medical billing services. We utilized state-of-the-art technology, the latest medical medical billing software and coding tools that helps us manage the entire billing cycle, ranging from patient registration to AR Collection with exceptional efficiency. We provide perfectly planned medical billing solutions and services.

Dedicated Billing Team
We assign a dedicated Billing Team to your account to handle all aspects of your billing needs — entering patient demographics, Verifying Insurance Eligibility, Review CPT/ICD-9 coding, entering charges, submitting claims, posting payments, sending patient statements, following up on accounts receivable and answering patient billing questions. These representatives functions as the primary contact with your practice.
Coding
We supply the most current CPT, ICD-9, and HCPCS coding expertise to minimize denials and unnecessary delays in reimbursement.
Billing
We submit both electronic and paper claims to all payers and handle third-party billing (including Worker’s Compensation, Motor Vehicle, Personal Injury and liens).
Claims Follow-up
We review all unpaid claims within 30-45 days of the initial billing date, appeal denials (bundling, medical necessity, etc.), resubmit claims for review when initial payment is inconsistent with typical doctor profile, and maintain managed-care contract profiles to assure proper reimbursement — a critical factor in maximizing collections.
Posting
We also post insurance and patients payments received to patient accounts (line item application allowing tracking of CPT reimbursement history). We post adjustments according to provider’s managed-care contract profiles, monitoring the profiles for reimbursement accuracy as outlined above.
Statements
And we’ll send monthly statements to patients and follow up on non-payment by phone and mail. The patient billing cycle includes multiple statements, followed by delinquency notices.
Monitoring Requirements
We advise physicians on any changes in HCFA requirements, CPT, and ICD-9 coding to achieve claim compliance for the fullest reimbursement for services.
Reports
We provide comprehensive monthly closing reports that typically include a summary of charges, receipts, adjustments, accounts receivable analysis, and multiple productivity reports. We will offer you a wide range of custom reports that will enable you to evaluate the unique structure of your practice. We will regularly consult with you to review your monthly reports.
Review
We assist in fee-schedule review and updates to maximize the practice’s profitability.
Setting up a New Practice/Credentialing
We provide the necessary tools to the physicians to set up a new practice. We help design new super bill and assist physicians practice for credentialling with new insurances.

Recent Comments